The following is a sample of a systematic literature review dissertation written by our proficient thesis and dissertation writers. You can get a similar dissertation paper written according to your preferences and instructions from Best Dissertation Writers.
Introduction
Research Background
Effective medication adherence is key for successful management and treatment of different health problems. Medication non-adherence is a significant public health issue, especially among hypertensive patients, since it can be difficult to persuade them to take medication without the manifestation of the symptoms. For instance, when the patient is prescribed with antihypertensive medication, they take it for some time and stop once they feel and report no more symptoms and their blood pressure has been normalised. Cardiovascular diseases accounted for 5,278.4 per 100,000 age-standardised disability-adjusted life years in 2016 in Nigeria, according to the Global Burden of Disease (GBD) (Gakidou et al. 2017). The top two major causes of disability adjusted life years and years of life lost (YLLs) worldwide are hypertension-related disorders (particularly, ischaemic heart disease and cerebrovascular illness) (Okubadejo et al., 2019). According to World Health Organisation (2002), hypertension is majorly asymptomatic and only diagnosed after a major organ failure or incidentally. Thus, it poses a risk to patients who are not aware of their condition.
Hypertension is characterised by a persistently elevated blood pressure in the systemic vasculature. Hypertension is the most prevalent preventable risk factor for cardiovascular disease, including ischaemic heart disease, congestive cardiac failure, cerebrovascular disease (stroke), atrial fibrillation, myocardial infarction, chronic renal disease, and peripheral vascular disease (Oparil et al., 2018). Worldwide, there are 3.5 billion adults with sub-optimal blood pressure values with estimates suggesting that 1 in 4 adults are reported to be diagnosed with hypertension (Forouzanfar et al., 2017). The Global Burden of Disease project revealed that poorly controlled blood pressure is the most significant risk factor that contributes to the global burden of disease and the evidence also suggests that hypertension increases the risk of all-cause mortality (Benziger et al., 2016, Zhou et al., 2018).
According to the National Institute for Health and Care Excellence (NICE) guidelines in the United Kingdom for the management of hypertension, two consecutive blood pressure readings of 140/90 mmHg or higher fulfils the diagnosis of hypertension (NICE, 2019). The NICE guidelines indicate that lifestyle interventions, anti-hypertensive therapy, and close monitoring of blood pressure and end-organ damage are the cornerstones of management of hypertension (NICE, 2019). Lifestyle modifications such as adopting a high-fibre, low-fat, and whole foods rich diet, undertaking moderate-to-high intensity exercise for at least 30 minutes thrice-weekly, and undertaking smoking cessation have been shown to be effective in optimising blood pressure in patients with hypertension (Aronow, 2017). The NICE guidelines indicate that antihypertensive therapy should be offered to patients who have persistent hypertension above 140/90 mmHg despite undertaking the aforementioned lifestyle interventions (NICE, 2019). Examples of antihypertensive drugs include beta-blockers (e.g., atenolol and bisoprolol), angiotensin-converting enzyme (ACE) inhibitors (e.g., enalapril and lisinopril), angiotensin-receptor blockers (e.g., losartan and valsartan), calcium channel blockers (e.g., amlodipine and nifedipine) and diuretics (e.g., frusemide and hydrochlorothiazide) amongst others (Musini et al., 2017).
Non-adherence is a common problem in patients with chronic diseases such as hypertension (Abegaz et al., 2017). Non-adherence is associated with increased healthcare costs, an increased rate of hospitalisations, and an over-utilisation of healthcare services (Straka et al., 2018). The World Health Organisation (WHO) defines adherence as “the degree to which [a] person’s behaviour corresponds with the agreed recommendations from a health care provider” (cited by Jimmy and Jose, 2011, p.155). The NICE guidelines defined adherence as the degree to which an individual’s actions correspond with the agreed recommendations by a healthcare provider (NICE, 2009). A review of the literature reveals that there are three main types of non-adherence to pharmacotherapy. These are primary non-adherence, non-persistence, and non-conforming behaviours (Jimmy and Jose, 2011). Primary non-adherence is defined as prescriptions which are written by healthcare providers, but not initiated. Non-persistence occurs when patients decide to stop taking medications after starting them without the advice of a healthcare provider (Jimmy and Jose, 2011). Finally, non-conforming behaviour involves skipping doses, consuming medications at inappropriate times, or even consuming medications at the wrong dosage.
The evidence suggests that blood pressure control amongst hypertensive patients is poor – only 60% of hypertensive patients achieve the therapeutic goals set out by their healthcare providers (Burnier, 2017). There are several reasons for non-adherence. One systematic review sought to explore these reasons and categorised them as follows – patient-related, medication-related, healthcare provider related, health care system related, and socioeconomic factors (Lee et al., 2018). According to DiMatteo et al. (2021), a number of factors may contribute to non-adherence to prescribed pharmacotherapy. They proposed that these factors could be: – the person may not understand what they have to do, lack the motivation to resolve their underlying diseases, lack a strategy for abiding by the prescribed pharmacotherapeutic regimen, or fail to recall information (DiMatteo et al., 2021). Specific reasons for non-adherence to prescribed pharmacotherapy include poor communication between healthcare providers and patients, poor knowledge regarding the prescribed drugs, poor understanding regarding the indications and adverse effect profiles associated with specific drugs.
Hypertension is the leading cause of morbidity and mortality in Africa and Nigeria (setting for this current study), which is the most populous country in Africa contributes to this disease burden. The global prevalence of hypertension is increasing, and the African continent appears to be the most affected region worldwide (Akinlua et al., 2015). One 2015 study found that the overall prevalence of hypertension in Nigeria was 29% (Adeyole et al., 2015). In contrast to this figure, the pooled awareness rate of this disease was only 17.4%. Researchers estimated that the number of hypertensive patients in Nigeria would increase to 39 million by the year 2030, with a prevalence of 30% (Adeloye et al., 2015). Akintunde and Akintunde (2015) further noted that social determinants of health may also contribute to non-adherence to anti-hypertensive pharmacotherapy amongst Nigerian hypertensive patients. One study found that patients with good medication adherence were more likely to be better educated and are from higher socio-economic classes compared to those with poor medication adherence.
This systematic review seeks to analyse the issue of medication adherence in Nigerian hypertensives. The systematic review has been chosen as the approach for this topic as it ranks highly in the hierarchy of evidence (Burns et al., 2011). In this regard, the Preferred Reporting Items for Meta-Analyses and Systematic Reviews (PRISMA) guidelines shall be used to guide the conduct of this systematic review (Selçuk, 2019). There is a need to address this research question for the following reasons. First, the level of non-adherence to anti-hypertensive pharmacotherapy in the Nigerian patient population is not well defined. Indeed, a review of the literature reveals a paucity of studies which elucidates the prevalence of non-adherence to hypertensive therapy in Nigeria as well as the reasons for this issue. Second, there has never been a more important time to conduct a systematic review on this topic – the prevalence of hypertension is increasing globally, and the African continent contributes to the global burden of hypertension more than any other region worldwide (DiMatteo et al., 2021). Third, the available studies provide conflicting results, recruited patients with varying demographic factors, studied different hypertensive therapeutics, and used varying measures of adherence (Adeyole et al., 2015; Akinlua et al., 2015).
According to Gascón et al. (2004), medication adherence is among the predictors of hypertension treatment success, whereas poor medication adherence, as well as a lack of information and understanding about hypertension, have been identified as some of the primary consequences of poor hypertension control, that has a direct effect on patients’ wellbeing. When drug adherence is low, the therapeutic benefits of the medication are decreased, and the overall efficacy of prescribed treatment is reduced. The reduced quality of treatment arises from a lack of commitment to pharmacological treatment for reduced efficacy and productivity in hypertension treatment. Poor compliance with antihypertensive therapy is a significant public health problem that leads to complications, injuries and hypertension-related fatalities (Ajayi et al., 2018).
Okwuonu et al. (2015) have identified factors that contribute to poor blood pressure regulation as patient-related obstacles, such as a lack of information about hypertension, unrealistic treatment standards, weak medication adherence, incomprehension of lifestyle change and failure to apply them (Okwuonu et al. 2014). Further, in their study, Boima et al. (2015) reported a high rate of medication non-adherence of 66.7%, which is different to the findings by Ibrahim et al. (2020), who reported a drop in non-adherence to antihypertensive at 56.6%. In the study by Boima et al. (2015), 56.6% of hypertensive patients were found on follow-up at Federal Teaching Hospital, Ido-Ekiti. This level of non-adherence, on the other hand, was higher than 17.2% in Enugu, South-East Nigeria, 24.2% in Port Harcourt, South-South Nigeria, 34.5% in Kano, North-West Nigeria, 46.4% in Abeokuta, South-West Nigeria, and 53.3% in Ilorin, North Central Nigeria. The results obtained by Boima et al. (2015) were also higher than those published in other African countries, with Kenya reporting 33.4% and Ethiopia reporting 50.3% of non-adherence to hypertensive medication. Awokola et al. (2016) reported a low adherence rate of 59.8% of the participants. This indicates that more than half of the diagnosed cases are non-adherent, thus resulting in the increase in the utilisation of healthcare services.
Akitunde and Akitunde, (2015), suggested that adherence to hypertensive medication increases in line with the length of time the person has been diagnosed with the condition. This result builds upon previous studies that showed that adherence is higher in elderly patients than in younger patients. Consequently, patients who utilised clinic reported a higher adherence level irrespective of the period one has been diagnosed with hypertension, a higher number of medications administered, and a relatively young age, as indicated by other studies as a predictor of non-adherence (Adisa, Ilesanmi, and Fakeye, 2018). This may be due to the specialised treatment and available information in a specialist clinic for the management of chronic diseases.
According to the study by Adisa, Ilesanmi, and Fakeye (2018), medication adherence in hypertensive patients was dependent on the period one had been diagnosed with the condition (the more years one has had hypertension the more they are likely to adhere to the medication) presence of comorbidity, socioeconomic status (financial ability which impacts their ability to buy medication continuously or pay their health insurance and the cultural practice) as well as held beliefs on the condition and medications. Osamor and Owumi (2011), however, indicated that only 51% of hypertensive patients are compliant because they believed hypertension is curable with herbal medication and thus there is no need for medication. Similar results were reported by Akitunde and Akitunde, (2015) who illustrated that adherence improved with years of diagnosis. There was reported high adherence among those who have had the condition for more than five years and have comorbidity as compared to those with less than five years, only diagnosed with hypertension or held a traditional belief over the medication or the condition. Adisa et al.’s (2018) findings are consistent with other studies by Boima et al. (2015) and Akitunde and Akitunde (2015) that reported high adherence among older patients.
The hypertension prevalence in adults in Nigeria has been estimated to be between 2.1 and 41.72 percent (Akinlua et al., 2015). The prevalence varies depending on the setting for the study, age, and sex. According to the literature, there is a high prevalence in urban areas as compared to the rural setting (Akinlua et al., 2015). The study also claims that Nigerian men are more prone to hypertension than their female counterparts, despite the fact that women reported poorer blood pressure management than men (Akinlua et al., 2015). According to Forouzanfar et al. (2017), hypertension is a leading cause of the world’s mortality and morbidity rates and Nigeria is not an exception as hypertension is reported as a leading cause of death (Akunne and Adedapo, 2019). These deaths, according to Akunne and Adedapo (2019), are related to the hypertension complication resulting from drug non-adherence. In addition, they further argued that not all people who are hypertensive are aware of their condition.
Bakere et al. (2016) examined the prevalence of hypertension and concluded that hypertension screening should be integrated into primary care diagnosis. They also reported that hypertension is commonly associated with comorbidity, which suggested that the prevalence rates was higher than reported because some cases were not reported. According to the report by Odili et al. (2020), 38% of adult Nigerians aged 18 years and above have hypertension. They reported that 60% of the participants with high blood pressure were conscious of their condition, a third were receiving treatment and 12% had their condition under control (Odili et al., 2020). The prevalence of hypertension ranged from 20.9% in the North-Central region to 52.8% in the South-East. According to Odili et al. (2020), hypertension was present in both urban and rural settlements. This contradicts the research results obtained by Boima et al. (2015), which indicated a high prevalence of hypertension in urban areas as compared to rural areas. However, urban residents were more knowledgeable about the disorder and received care for it than their rural counterparts.
The diagnosis of hypertension can be depressive, especially with the fear of the potential prognosis. Osamor and Owumi (2011) argued that holding certain beliefs about medication was an influencing factor for medication compliance. The study illustrated that the community believed that the use of orthodox and herbal medication cures hypertension, thus explaining why they did not adhere to the prescribed medication. The study further illustrated that patients with monotherapy were more compliant than those with multiple medications. The findings by Adisa et al. (2018) were different to those of Osamor and Owumi (2011) who reported a high adherence rates in a monotherapy. Adisa et al. (2018), however, argued that patients with at least two types of medication reported a high adherence rate as compared to those prescribed with a single medication. Boima et al. (2015) argued that concerns about becoming dependent and a lack of knowledge regarding the curability of hypertension were associated with medication non-adherence. The findings by Okwuonu et al. (2014), in return, illustrated that medication adherence is attributed to patient-related challenges such as a lack of information about hypertension, unrealistic treatment standards, weak medication adherence, incomprehension of lifestyle change and failure to apply them.
Akunne and Adedapo (2019) argued that the prescribed medication impacts the patients’ adherence or non-adherence behaviour. The study highlighted that the combined prescriptions increased non-adherence as compared to a single therapy. The research further indicates that the different prescriptions have different costs and thus, costly medication are more prone to not being purchased, especially for those who have to pay for the medication themselves. In their study, Okwuonu et al. (2014) agreed with the aforementioned assertion by indicating that patients with multiple prescriptions either forget to take all their medicines or do not remember to carry them during the day when they left their homes. Awokola et al. (2016) have asserted that patient-related factors are the major contributors to non-adherence. The study reported that lack of funds to purchase medication, forgetfulness, the availability of herbal remedies, spiritual healing, which can be promoted by the spiritual leaders, and misinformation about the seriousness of the condition are the main factors contributing to the patients’ non-adherence.
Odiase and Ogbemudia (2019) observed that the development of another condition could result in the non-adherent of antihypertensive medication. They reported that more than 30% of stroke survivors became non-adherent after a few months after experiencing the stroke. Akinlua et al., (2018), reported that the beliefs held by public health careers on hypertension with regards to the management and curability of hypertension can impact on patients’ adherence to medication. They reported that these public health careers pass the information to the patients based on what they know; thus, there is a need to have a clear education concerning hypertension to enable them to correctly inform the patients.
Literacy levels have been demonstrated to impact the adherence level of the hypertension level. Osamor and Owumi (2011) indicated that the patients did not have adequate knowledge concerning the nature of hypertension and thus impacting their decision. Boima et al. (2015) agreed and stated that an increase in literacy levels among Nigerians has had a positive impact on adherence, albeit of low significance. Consequently, another study by Kazaure et al. (2017) indicated that drug adherence is associated with social factors. In the research, younger civil servants were significantly more likely than senior civil servants to be non-compliant. One potential explanation is that junior civil servants have lower salaries than senior civil servants, and possibly cannot afford to purchase these medications. In addition, as opposed to senior civil servants, junior civil servants are younger. Previous research by Adisa et al. (2018), Boima et al. (2015), and Akitunde and Akitunde, (2015) has established that older patients are more likely to adhere to their medication regimens. Patients who ran out of their medications before their next doctor visit were more likely to be non-adherent than those who did not (Kazaure et al., 2017).
Boima et al. (2015) found that patients who were not adhering to the treatment plan were younger than those who demonstrated adherence. One possible cause is that older patients are more worried about their health than younger patients and they receive enough counselling about the consequences. In comparison to Akitunde and Akitunde, (2015), non-adherence in the young patient is related to the shorter period form diagnosis of the hypertension. Contrary to this, Ibrahim et al. (2020) have indicated that the increase in the duration of the condition and age did not impact adherence of hypertensive medication.
Another study by Akintunde and Akintunde (2015) evaluated the adherence to hypertensive medication as well as the determinants concerning the place of care. The findings illustrated that the patients who attended the clinic at the specialist’s centre had a higher adherence rate as compared to those who went to the general public clinics. The study indicates that the difference in social-economic status impacts the place where individuals seek care. Akintunde and Akitunde (2015) further observe that the high adherence among the patients who attended specialist clinic resulted in receiving personalised and focused care. According to Akunne and Adedapo (2019), Nigerians’ socioeconomic status is still low compared to other Africa nations such as South Africa and the western world, with many people living below the poverty line. The study indicates that financial constraints prevent them from meeting their basic needs such as health needs and food. This prevents individuals from consistently purchasing their medication, especially when they do not have health insurance and depend on it out of pocket. The findings agree with a previous study by Adisa et al. (2018), which identified the cost of medication as an impeding factor as not all patients could afford the medication prescribed for them.
Oluwole et al. (2019), on the contrary, argued that there is no correlation between medication adherence and patient satisfaction and thus patients’ counselling and education should be enhanced to support the acquisition of positive outcomes. According to the study by Adeyemo et al. (2013), patients were involved in a 6 month randomised trial. The findings indicated a 77% adherence rate with higher non-adherent being reported among the rural dwellers than in urban areas. Odili et al. (2020) agreed by illustrating that hypertensive patients in urban areas were more knowledgeable about the condition compared to rural dwellers. The study points to access to primary care facilities as an underpinning factor as it hinders some patients from consistently attending their clinics.
Problem Statement
As discussed above a number of research studies have investigated on the predictors of antihypertensive medication adherence, though they are primarily quantitative in nature. Quantitative research reveals trends in a large population but does not evaluate participants’ deep emotions or feelings towards a topic as qualitative research could and thus one cannot determine to what extent the predictor’s impact on individuals at the individual level. Also, 80% of the studies are concentrated in the western region of Nigeria, which has two ethnic groups (Yoruba and Hausa). This raises the need to carry out similar research in other regions due to the difference in culture and ethnicity to determine if the same findings will be drawn. Lastly, all the studies undertaken relied on the Morisky medication adherence scale (MMAS), which raises the concern about the acquisition of different results if other scales were used or a combination of scales. The addressing of the identified gaps is essential for drawing an effective conclusion and implementation of the necessary interventions to improve healthcare delivery and outcomes. This systematic review will explore studies conducting on hypertensive medication adherence in Nigeria, which have recruited different groups of people, using different methods of assessing adherence, with patients using different medications. The findings will be used to inform future research as well as interventions to address hypertension medication adherence.
Research Question
- What is the prevalence of non-adherence to pharmacotherapy in Nigerian adults with hypertension and what factors influence non-adherence?
Research Objectives
- To delineate the prevalence of non-adherence to anti-hypertensive therapy in Nigerian hypertensives.
- To delineate the reasons underpinning non-adherence in this specific patient population.
Research Method
Introduction
This chapter details the underpinning epistemological position of the researcher before mapping the study’s overarching methodological approach and the systematic review utilised. The study’s goal was to find how often medication non-adherence is among Nigerians with hypertension, as well as the factors that contribute to non-adherence. Findings from this review will provide information for evidence-based strategies for improving adherence to hypertensive medication in this population.
The chapter will firstly outline the positioning of the research and researcher within an available evidence stance. It will be followed by considering the overarching case study methodology based on Hellwick (2015) and Yin (2014) and the adoption of a systematic review. To underpin the empirical work, the initial phase focused on a scoping review of the available evidence, mapping the evidence-base and clarifying the research questions aligned to develop a series of theoretical propositions to guide a subsequent systematic literature review (Yin, 2014). The methodology and implementation of the systematic review phase provided the platform for grounding the emergent findings in an applied practice context, focused on stakeholder engagement.
Study Design
The study adopted a systematic review research strategy. The factors that influence hypertension medication non-adherence in adult Nigerians were investigated using a systematic review. This systematic review analysed studies retrieved from two databases to find a diverse range of papers, then used inclusion and exclusion criteria to find the most relevant studies on the factors that influence medication non-adherence (Suri, 2020). In various respects, systematic reviews differ from typical narrative reviews. As the name implies, systematic reviews usually employ a thorough approach and search procedure devised a forethought with the purpose of decreasing bias by locating, analysing, and consolidating all relevant literature on a given issue (Roberts, 2006).
The systematic review was chosen over qualitative and quantitative research approaches due to its ability to produce more relevant and reliable literature concerning the research question (Cerigo and Quesnel-Vallée, 2020). According to Pollock and Berge (2018), a systematic review is an essential way to keep up with the ever-growing pool of evidence necessary for quality of care improvement. The growth in healthcare, nursing, and associated medical practitioner writing in the later part of the twentieth century, which has continued far into the new millennium, has made keeping up with existing primary research unfeasible (Green et al., 2011). The use of primary sources raised pedagogical challenges due to the sampling and the minimal number of participants involved (Cleary and Neumann, 2009). There has also been a surge in online access to articles, resulting in a sometimes-great quantity of hits to sift through. Furthermore, there is the problem of developing and maintaining skills in using a wide range of electronic devices that provide access to vast volumes of data (Hewitt et al., 2008; Torgerson, 2006).
Furthermore, physicians, nurses, mental health professionals, hospital administrators, policymakers, and patients all have varied information needs, for example, high-quality data on the efficacy, importance, practicality, and appropriateness of a wide range of healthcare initiatives (Green et al., (2011). Many people’s busy clinical or professional schedules are disrupted by this necessity. The quantity of information available to consumers (patients) can be confusing, and an absence of technical skills can lead to incorrect information being believed, increasing healthcare professional workload and putting patient safety at risk (Green et al., 2011).
It is not uncommon for the number of published studies in a particular field to reach the hundreds or even thousands (before being filtered for inclusion in a study). When the content is read, most of these studies may produce unclear, ambiguous, or conflicting data; they might not have been published in English, or there may be a misunderstanding about whether the outcomes can be applied in any country (Bastian, 1994). Each article may provide little insight into the topic when evaluated individually. Nevertheless, when reviewed altogether as part of the comprehensive review, a more coherent image should materialise.
According to Shea et al. (2001), systematic reviews are required to determine the practicality and cost-effectiveness of a treatment or medicine. Multiple technology assessments and single technology assessments are fundamental to the National Institute of Health and Clinical Excellence’s health technology assessment process. Systematic reviews, on the other hand, are the most useful when there is a fundamental question, numerous main studies – maybe with contradictory findings – and some uncertainty.
It necessitates a clear statement of the review’s objectives, the remedy or phenomenon being studied, appropriate patient groups and subpopulations (and, in some cases, delivery sites), the kind of evidence or studies that will be used to answer the question, and suitable results. These details are used to reduce the number of publications considered for inclusion in the review. A PICO statement was used to state a systematic review and develop the research question; it will be utilised to determine the efficacy of an intervention in this study (Ranganathan and Aggarwal, 2020). The standardised Population, Intervention, Comparison, and Outcome (PICO) paradigm was used to evaluate the stated research question to create key search words for this systematic review (Schardt et al., 2007). The deconstruction of the research question is illustrated below.
- P: Nigerian hypertensive
- I: Use of medication (pharmacotherapy)
- C: Not applied
- O: Non-adherence or adherence in patient
Literature Search Strategy
The required research relevant to an intervention or activity was carefully searched in the published and unpublished literature (reporting the outcomes correctly and with the right patients). The investigation attempted to cover all literature to provide an unbiased assessment. In actuality, only a small percentage of databases are searched using a standard or customised search filter. Specialised search engines, databases, and websites are also used to look for grey literature (information that has not been formally published, such as technical reports or institutional, conference proceedings, working papers or other documents that are not normally subject to editorial control or peer review). Expertise advice was sought on where to find relevant data, and major authors were engaged for clarifications. When appropriate, selected publications were hand-searched, just as the references of full-text papers. Publication bias, selection bias, and language bias are all possible biases in this research (Dubben and Beck-Bornholdt, 2005). It was as a result of the specified research question to be answered that had to include only studies concerning the Nigerian population, hypertensive medication adherence related and within the inclusion and exclusion criteria bracket of the year of publication.
Two online scientific databases were used for the systematic review. PubMed and EMBASE are the two databases. The search phrases ‘Nigeria *’, ‘hypertension’, and ‘adherence’ will be utilised. To account for word expansions such as’ Nigerians,’ the search phrase ‘Nigeria *’ has been abbreviated with an asterisk. The keyword “non-adherence” was removed from the search since the phrase “adherence” will have the same findings. To aid the search method in providing satisfactory results, Boolean operators such as “AND” and “OR” were used. According to the research, combining the use of strategically chosen search keywords, truncations, and Boolean operators is a reliable method (Ecker and Skelly, 2010).
Keywords and Search Terms
Three key search terms were developed to limit the sources retrieved from the databases used (Nigeria, hypertension and adherence). Nigeria was used to restrict the geographical boundaries to the population of interest as the study question refers only to the Nigerian adults. Hypertension was also used as a search term as it is the condition of interest in the study. Its use eliminated other conditions from being retrieved from the search. Adherence was used to justify the intended outcomes; its use helped retrieve studies with non-adherence and non-adherence rates among the population. To retrieve relevant sources, the search terms were combined in the search engines with Boolean operators “and” and “or”.
Inclusion and Exclusion Criteria
Before the sources were screened, certain limiters were set on the user interfaces of the PubMed and EMBASE online scientific databases. To begin with, results were limited to the year of publication, with only research published within the last ten years being considered for review due to the systematic review’s desire to be current and relevant to clinical settings. Second, only papers that were fully published in English were considered. As a result, our evaluation did not include abstract-only research or conference displays lacking supporting materials. There was no restriction on geography because the keyword Nigeria effectively excluded papers from outside the country. The lowest age range was similarly set at 18 years old since the systematic literature review was limited to adults exclusively.
After removing duplicates, the remaining results will be vetted by looking over their titles and abstracts in order. After removing duplicate findings from the search engines, full-text articles from the remaining results were verified for relevance and authenticity to the research question. The papers were screened and filtered according to Selçuk’s (2019) Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards. The articles which were not appropriate to the research objective were eliminated, and the publications that remained were thoroughly examined using an abstract analysis. Studies were submitted to a strict set of eligibility criteria during the comprehensive analysis. The articles included were reflective of the Nigerian population, adult hypertensive patients, and managed with medication. Consequently, studies about hypertension medication adherence but not reflective of the Nigerian population were also excluded. The research was on hypertension and not involving disabling comorbidities such as stroke. These inclusion and exclusion criteria used for the included sources is Tabulated as below.
Table 1: Inclusion and exclusion criteria
| Inclusion Criteria | Exclusion Criteria |
| Studies entailing Adult Nigerian hypertension patients (18 years and above). | Not published in English or full text |
| Hypertension patient on medication therapy | Hypertensive studies involving disabling co-morbidities such as severe stroke |
| Studies with a validated medication adherence measurement tool | Hypertensive studies involving children |
| Cross-sectional studies | Case series, case studies, systematic reviews, observational studies, or meta-analyses |
| – | Studies involving HIV patients |
| Published before (2011) |
The primary outcome of interest was adherence to pharmacotherapy in Nigerian hypertensive patients. Secondary outcomes include reasons for non-adherence to antihypertensive therapy in this patient population.
Quality Assessment
After the exposure of the identified sources to the inclusion and exclusion criteria, the sources were further evaluated for quality. The CASP checklist was used to determine the reliability and validity of the sources. On assessment, only sources that scored more than six (out of the maximum of 10) were included in the review because the sources which scored below six had limited quality and thus could negatively impact the findings of the study.
Data Synthesis
In this study, thematic analysis was used. Because the chosen literature was quantitative and qualitative studies, it was essential to analyse them using emergent themes. As a result, the researcher created codes comprising repetitive or related terms, assertions, and conclusions to extract the overall themes from the selected studies. To develop generic themes, comparable codes were grouped. The different generated themes were then discussed and a conclusion drawn that will be used to inform future research. Using meta-synthesis, the research used the retrieved information and identified themes to develop new theorise and interpretations on the factors influencing non-adherence of hypertensive medication among Nigerian adults.
Ethics
Compared to qualitative research, the systematic review does not involve the collection of personalised data. The systematic review is based on publicly available sources in collaboration with institutional ethical approval. The study topic does not infringe the ethical standards of any person as it did not involve the collection of primary data. Nevertheless, conducting a systematic review is prone to plagiarism due to the use of other researchers’ findings without their consent and not acknowledging their input. To avoid the ethical concern of plagiarism, all the information used in the research and not of the researcher’s own opinion is adequately cited to acknowledge and give credit to the works of the different researchers. Another ethical concern that could arise is the selection bias and the methodological bias. To avoid this issue, the current research involved both quantitative and qualitative research in the review. Systematic researchers must ethically assess how their context orientation shapes the interconnected knowledge and understanding they are developing from the filtered data through informed subjectivity and reflexivity (Suri, 2020). It allowed the researcher to draw a conclusion and thus develop a reliable rationale. Another ethical issue is the conflict of interest (Vergnes et al., 2010). The use of systematic review relay on the published material, and thus the inclusion of unethical sources can result in the publication of unethical findings, which is a drawback of a systematic review.
Results
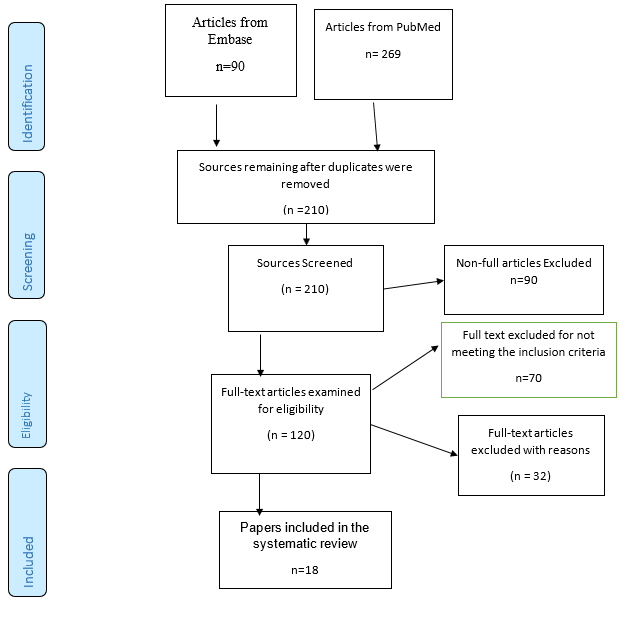
A sum of 369 articles was retrieved from the two databases used. A total of 279 were from PubMed and 90 from Embase. The articles were further evaluated where 159 were excluded due to duplication. The remaining 210 were further evaluated, and 90 were removed for not being full articles. The remaining 120 articles were further screened for validity and reliability for answering the research question. Through exposure to the inclusion and exclusion criteria, 70 more articles were excluded from the review. The remaining 50 articles were assessed for eligibility; 32 articles were further removed with reasons. The remaining 18 sources were included in the review and represented in the literature review matrix in the appendix. The sources included were both qualitative and quantitative to expand the data on adherence in Nigeria. Poor medication adherence is a significant public health issue, especially among hypertensive patients, since it can be difficult to persuade them to take medication without the manifestation of the symptoms. The included studies are illustrated in the PRISMA diagram Table 1, while the excluded sources with reasons are illustrated in Table 2.
Figure 1: PRISMA Flow Chart illustrating the study selection process
Table 2: Reasons for exclusion of full text
| Number of sources excluded | Reasons For exclusion |
| 6 | Inclusion of other countries |
| 2 | Lack of results |
| 8 | Use of combined intervention (mediation, exercise, diet) |
| 2 | Undisclosed sample size |
| 1 | Wrong publication date |
| 3 | Too small N |
| 2 | Inclusion of Stroke patient |
| 4 | Diabetic patients with hypertension |
| 1 | Lack of clear research design |
| 1 | Inconsistence in the results reporting |
| 2 | Study population |
Characteristics of the Sources
The data extraction process entailed the review of all the 18 sources identified. The review sought to identify themes relevant to answering the research question, determining the adherence levels and the factors impacting the reported adherence in the different studies. Both statistical features reported in the study, as well as the observational factors, are reported under this section. Of the identified factors for non-adherence, forgetfulness was reported in most of the studies and thus the major problem among the population. The data extraction process led to the acquisition of the results as discussed below:
The systematic review participants in the studies were a total of N (6804) respondents. The smallest sample size was 40, while the largest was 1050, with most studies having at least 400 participants. The eighteen sources reviewed identified different adherence and non-adherence rates with contributing factors as indicated in Table 4. The highest non-adherence rate being 95.6%, while the lowest non-adherence being at 8.9%. Similarly, one study reported a high adherence rate at 85.5%. The high adherence indicated that when measures are put in place, most of the patients can be adherent to the medication and thus an improved quality of life. The overview of the sources, representation of the different genders, sample size and the period of study is illustrated in Table 3 in the appendices.
Medication Adherence
Medication adherence is discussed by different sources, illustrating the levels of non-adherence as well as the factors contributing to high rates of adherence. Okwuonu et al. (2014) and Ibrahim et al. (2020) agree that there are high non-adherence rates in Nigerian adults between eighteen to eighty-five years. Despite the agreement, the sources illustrate different rates and causes of non-adherence. Ibrahim et al. (2020) reported a reduction in the non-adherence rates to 56.6% from 60.8%, as reported by Usman et al. (2019). Adherence is also reported to be affected by the duration one has been diagnosed with the infection. Thus, high adherence rates are found in older patients compared to young ones, according to Iloh et al. (2013). Odiase and Ogbemudia (2019) discussed adherence in relation to educational qualifications and concluded that adherence is unrelated to educational level. Adherence is also reported to be affected by the duration one has been diagnosed with the infection. Iloh et al. (2013), identified factors for non-adherence, such as medication side effects, feeling better, forgetfulness and use of herbal remedies as discussed in detail in this section.
Usman et al., (2019), study included a total of 237 hypertension individuals. The participants’ average age was 40.5 years (SD=10.3 years), with a range of 23 to 64 years. 161 (67.9%) of the participants were female, 119 (50.2%) were Nupe ethnicity, and 120 (50.6%) were between the ages of 40 and 60. More over two-thirds of the respondents were married (79.7%), and 93 (39.2%) were working. The overall medication adherence of the subjects was 39.2 percent (n=237). Adherence to medication was higher in females (52.7%) and younger participants (74.2%). Adherence was also higher in those who took three medications (73.1%) and those who got pharmacist coaching (82.8%).
Odusola et al., (2014) study entailed 40 participants. Half of them had managed blood pressure (systolic 140 mmHg and diastolic 90 mmHg), whereas the other half had unregulated blood pressure (systolic 140 mmHg and/or diastolic 90 mmHg). The majority of the people were above the age of 50. All were from rural areas, with 80% earning less than $5 a day, 70% having no or only a primary school education, almost all (92%) living in substandard housing, and the majority (75%) working as farmers, artisans, or traders. All were religious, with 62.5 percent of Christians and 37.5 percent of Muslims. Some patients admitted that they did not always take their prescriptions as prescribed. Trends of “self-regulation” that were frequently cited included lowering daily dosages, skipping prescriptions under certain conditions, and stopping medications for days or weeks. The participants cited the medication side effects, healthcare dissatisfaction, lack of social support and religious belief as contributors of non-adherence.
As stated by Okoro and Ngong (2012), the majority of responders, 115 (75.7%), take their drugs exactly as recommended, while 37 (24.3%) do not. Medications cost, (3.9%), busy work schedules and nature of the profession, treatment side effects and feeling worse (6.6%), forgetfulness (1.3%), and feeling better (5.3%) were cited as factors for not adhering to their medications as prescribed. Compared to Awokola et al. (2016), Okoro and Ngong (2012) reported lower non-adherence at 24.3% up to 59.8%. The far more prevalent causes of drug non-adherence, according to the study, were discontinuing prescriptions when feeling worse and well. At the same time, Awokola et al. (2016) reported the lack of financial ability as the highest cause for non-adherence. The study reported a high adherence rate, though it was observed that adherence to the medication is not correlated to controlled blood pressure. The findings of the review point to the need for enhanced education. Patient education will adequately inform patients about the nature of the diagnosis and the significance of adherence, as medication adherence correlates with blood pressure control.
In comparison to Akintunde and Akintunde, (2015) a little over half of those attending the GOPD clinic, more than four-fifths of those attending the cardiology clinic had at least a medium level of adherence. Those who adhered well were more likely to be older, have a greater degree of education, and earn more every month than those who did not. Ezeala-Adikaibe et al. (2017) also reported that increased knowledge is associated with high adherence among hypertension patients. The findings indicate that patients who received effective counselling and patient education during their routine clinics reported a high medication adherence rate. Despite a shorter hypertensive duration, a large number of medicines prescribed, and a younger age, the specialised clinic appeared to be related to a higher level of adherence (Akintunde and Akintunde, 2015). The study asserts the importance of a patient-centered approach to managing hypertension. This is because the young and recently diagnosed patients attending specialty clinics reported high adherence rates compared to those attending general primary care services due to the difference in approach used by the practitioners in the two facilities. Adeoye et al. (2019) further agreed by illustrating that the increase in patient knowledge was reflective in the reported adherence rates and thus the need for enhanced patient education.
Iloh et al. (2013) investigated hypertension patient medication adherence in 140 participants. The hypertension patients ranged from 32 to 83 years old, with a mean age of 52 ± 7.4 years. With a male to female ratio of 1: 1.5, there were 56 (40.0%) males and 84 (60.0%) females. Ninety-eight patients (70.0%) had been hypertensive for less than three years, while 42 patients (30.0%) had been hypertension for three years or more. Twenty-nine (59.2%) of the 49 individuals with good blood pressure control had been hypertensive for three years or more, while 20 (40.8%) had been hypertensive for less than three years. The difference between the two groups was statistically significant (p-value = 0.042; Chi-square = 3.18; df = 1). Out of 140 patients, sixty (42.9%) were adherent, whereas the remaining 80 (57.1%) were not. 45 (91.8%) of the 49 patients with good blood pressure management were adherent, while 4 (8.2%) were not. When compared to non-adherent patients, those who adhered to antihypertensive treatment had significantly better blood pressure management (Chi-square = 5.12; df = 1; p-value = 0.03). The most prevalent cause given by hypertension patients for non-adherence to prescriptions was forgetfulness (32.4%). Other factors were a sense of well-being (25.6%), a lack of cash (25.6%), spiritual leaders’ recommendations (8.7%), and herbal cures (7.7%). This small change was statistically meaningful (p-value = 0.046; Chi-square = 6.03; df = 4). The reported non-adherence rate of 57.1% was closely related to the adherence rate reported by Awokola et al. (2016) at 59.8%. Iloh et al.’s (2013) findings agree with those reported by Okoro and Ngong (2012), Awokola et al. (2016) and Adisa et al. (2018) on factors of non-adherence being forgetfulness, cost of medication use of herbal medicine and feeling well or worse.
Adisa et al. (2018) studied hypertensive patients (n = 605) at two tertiary healthcare institutions. Within the study period, 624 patients were solicited for participation, with 605 consenting and completing the trial, for a response rate of 97%. Females accounted for 358 (59.2%) of the total, while males accounted for 247 (40.8%). The average age was 54.5 11.4 years, with the majority of 348 people (57.5%) between 40 and 59. Forty-three patients (7.1%) were diagnosed for less than a year, 430 (71.1%) for one to five years, 122 (20.2%) for six to ten years, and ten (1.7%) for eleven to fifteen years. In all, 473 people (78.2%) had hypertension for less than 5 years, and 132 (21.8%) had it for more than 5 years. According to the modified Morisky Adherence Predictor Scale, 54 patients (8.9%) had total scores of 1 indicating optimal antihypertensive medication adherence, whereas 551 (91.1%) had scores of > 1 indicating non-adherence. Forgetfulness (404), dose omission (370), side effects (157), non-affordability of medication costs (95), dislike of the medication (74), deliberate decision to take medication when desired (34), and preference of her doctor were all mentioned as reasons for non-adherence to prescribed medications. Participants with at least high-school education adhered to their medications substantially better than those with only elementary school education.
In addition, when compared to individuals on monotherapy, adherence is much higher among patients on at least two medications. Patients with hypertension for less than 5 years had greater medication adherence (66.7%) than those with hypertension for more than 5 years (33.3%) (Chi-square = 4.61, p = 0.032). The study by Adisa et al. (2018) emphasizes the impact of forgetfulness by rating it as the highest factor for non-adherence. Therefore, such outcomes show that non-adherence arising from forgetfulness has been on the rise. Iloh et al. (2013) reported forgetfulness at 32.4%, and the levels have been reported to escalate year after the other. It is illustrated by Ezeala-Adikaibe et al. (2017) study, which reported that 94.3% of the non-adherence cases resulted from forgetfulness where the patient did not pack their medication, missed a dose or did not carry all their medication for those prescribed with more than therapy. Similar to Adisa et al. (2018), Okoro and Ngong et al. (2012) had earlier identified the cost of medication as a contributing factor for non-adherence, though at a low level. The increase in the identification of the cost of medication as a contributing factor for non-adherence is associated with the poor living standards of the Nigerians, unemployment and general low social-economic standards.
Ezeala-Adikaibe et al.’s (2017) study of 436 patients was investigated. The majority of patients (90.1%) forget to take their medicines; 94.3% forget to pack them with them when they leave home. Patients who were completely reliant on others had the highest rates of non-adherence (62.5 %). Non-adherence was linked to high depression scores, low disability ratings, and the existence of peptic ulcer illnesses. The study also indicated that patients who have had the condition for a longer time recorded high levels of depression and similarly high non-adherence. The study found that older patients were less likely to take their medication because they were overly reliant on social media. Consequently, social network reliance was indicated to increase non-adherence in patients who had minimal support. Ezeala-Adikaibe et al.’s (2017) findings support those reported by Osamor and Owumi (2011), Adisa et al. (2018), Iloh et al. (2013) and Ayodapo et al. (2019), who indicted the importance of social networks and the role they play in reminding the patients of their medication as well as financial support to ensure the medications are continuously filled. Death (n=7), severe cardiovascular events (two strokes and one congestive cardiac failure), referrals caused by unforeseen high blood pressure (n=11), treatment side effects (excessive micturition, dizziness, etc.) (n=9), loss of interest in engagement (n=5), and choice of alternative medicine (n=3) were the known reasons for non-completion.
Overall, adherence was strong among patients who completed the 6-month study (77% took > 98% of prescribed medications). Pill counts were used as the primary adherence indicator, while a biological assay using a urine riboflavin tracer was used as a secondary adherence indicator. At each clinic appointment, pill counts were taken; patients returned all drugs, and the counts were documented. The proportion of medications consumed, divided by the total of tablets prescribed during the evaluation period, was used to calculate pill count adherence. In the study, it was only possible to measure adherence to persistence in the taking of the pill, other than compliance, as it was not possible to determine the number of pills taken at the prescribed time. Each subject was asked to take 50 mg of riboflavin daily with their morning dosage of antihypertensive medication for the biological assay assessment. Under UV light, a single dose of 50 mg riboflavin could be reliably detected in urine for 18–24 hours. Adherence was not affected by the treatment arm. However, it was better in rural than in urban areas and with a greater baseline blood pressure. After 6 months, 66% of individuals had achieved hypertension control (blood pressure of less than 140/90 mmHg). The study does not identify the patient-related factors for adherence nor adherence but was able to determine the level of adherence in the studied sample.
The observed association between medication adherence and treatment satisfaction was doubtful to be related to unmeasured confounding factors, according to sensitivity analysis. Medication adherence was poor, and treatment satisfaction was seen to result in increased medication adherence. The outcomes from Ezeala-Adikaibe et al. (2017) show that patients with positive treatment satisfaction rates had higher hypertension medication adherence. Satisfaction was associated with the absence of medication side effects, the medication being within the affordable cost and prescribed at a convenient time for the patient. Some research indicated that patients preferred an evening dosage, single, and multiple dosages, while some pill bulkiness reinforced their non-adherence. Iloh and Amadi (2017) also argued that patients’ adherence was associated with their reported satisfaction with the treatment.
Iloh and Amadi’s (2017) study to determine the relationship between satisfaction and adherence found that patient satisfaction was an independent predictor of medication adherence among hypertension patients. The study participants ranged in age from 32 to 83, with an average age of 52.74 years. There were 56 (40.0%) men and 84 (60.0%) women in the group. Treatment satisfaction, medication adherence, and blood pressure management were at 78.6%, 42.9 %, and 35.0 %, respectively. Treatment satisfaction was found to be linked to medication adherence (p = 0.01) and blood pressure control (p = 0.031). In the study of 140 hypertensive patients, 110 (78.6%) were content with the antihypertensive treatment they received, whereas 30 (21.4%) were not. Furthermore, 60 (42.9%) of hypertension patients took their antihypertensive medication as prescribed, while 80 (57.1%) did not. Moreover, 49 (35.0%) participants had good blood pressure control, while 91 (65.0%) reported uncontrolled blood pressure. 56 (50.9%) of the 110 patients with hypertension who were content with their therapy were medication adherent, whereas 54 (49.1%) were pharmaceutical non-adherent. Conversely, 56 (50.9%) of the 60 (42.9%) hypertension patients who were medication compliant were content with their therapy, while 4 (13.3%) were unsatisfied with their care. The variation (Chi-Square = 13.61; p = 0.01) was significant statistically. As stipulated by Akintunde and Akintunde (2015), patients who attend specialised clinics reported a high adherence rate compared to those who attended the general primary care adherence. The difference was also evident in their medication adherence rates, where the general clinics’ rates were lower than those attending the specialty clinics. In the analysis of the results reported by Iloh and Amadi (2017), non-adherence among the studied population is attributed to the patient’s perceived satisfaction with the treatment. The treatment’s convenience, continuity, and flexibility were used to gauge satisfaction. The study also highlights the complexity of comorbidity, which leads to a complicated medication regimen and, as a result, lower adherence rates. Akintunde and Akintunde (2015) identified the importance of the time used for patient counselling as more time used was more efficient in enhancing adherence rates.
A study by Okwuonu et al. (2014) had a total of 252 people taking part in the study, including 143 men (56.7%) and 109 women (43.3%). The participants’ average age was 56.6 + or – 12.7 years, and they had been diagnosed with hypertension for an average of 6.1 to 3.3 years. According to the Joint National Committee on Prevention, Detection, and Evaluation of High Blood Pressure’s Seventh Report, 32.9 % of these individuals had regulated blood pressure. In comparison, 39.3 % and 27.8 %, respectively, had stage 1 and stage 2 hypertension. Only 23.4 % were aware of the effects of inadequate blood pressure control, and 64 % expected medication to cure hypertension even when the reason was unknown. Okwuonu et al. (2014) indicated that 68.7% of the study participants had poor medication adherence, with causes ranging from forgetfulness (61.2 %), financial restrictions (56.6 %), significant pill burden (22.5 %), pharmaceutical side effects (17.3%), and reduced recorded blood pressure (12.1 %). Furthermore, people do not understand or practice the lifestyle changes required for blood pressure control. Illustration, current research argues that there is a reported lack of adequate patient education, which greatly influences the increase in medication non-adherence.
Oluwole et al. (2019) conducted a study with 500 participants, the average age being 58.9 13.3 years. The majority of the respondents in the research had ‘moderate’ adherence to antihypertensive treatment (446 [89.2 %]). Only five people (1.0 %) said they had a “strong” level of adherence. All satisfaction domains, including the overall domain, had the highest mean ratings in the moderate adherence category. Treatment satisfaction was statistically meaningful (p = 0.000) in its relationship with medication adherence. The patients perceived treatment as satisfactory if convenient for them, at an affordable cost, and the intervention improved their feelings. In this study, one out of every hundred patients had a high level of adherence to hypertension medication, and there was a link between treatment satisfaction and adherence to medication.
Ayodapo et al. (2020) study investigated hypertension medication adherence among patients attending a tertiary primary health facility. The average age of the participants was 60.97 + or – 11.28 years, with a small female majority (1:1.7 male: female). Three hundred and forty-nine people (83.1%) were married, 273 (65.0%) came from monogamous families, and 375 (89.2%) had families of more than four members. 94% (22.4%) had a strong understanding of hypertension, and 257 people (61.2%) took their medication as prescribed. As awareness of hypertension increases, an increase in drug adherence has also improved. Subjects with strong knowledge have a 2 times better chance of sticking to their treatment (OR = 2.320, 95 % CI = 1.164, 4.626) than those with weak knowledge. Ayodapo et al.’s (2020) findings support those earlier reported by Adeoye et al. (2019), which identified knowledge and motivation as predictors of adherence among hypertension patients.
The study by Adeoye et al. (2019) evaluated the adherence levels among hypertensive patients. The average age was 61.33 years old, and the average blood pressure was 158/91 mmHg. High adherence was observed in 4.1 % of the individuals, while medium and low adherence were identified in 68.9% and 27% of the participants, respectively. A third of the participants had real uncontrolled hypertension. A large percentage of the study participants also had a high level of motivation (68.9%) and knowledge (89.2 %). Motivation (p = 0.0001), knowledge (p = 0.002), and obesity (p = 0.036) were all linked to adherence to medication. Knowledge was an independent predictor of drug adherence, but it did not influence blood pressure control. Concerning Adeoye et al. (2019), the study found that patients who were motivated and well informed about their condition were more adherent to the prescribed medication. The study agrees with the works by Iloh et al. (2013) and Ibrahim et al. (2020) on the need for improved patient education in various health facilities to increase medication adherence. Adeoye et al. (2019) also indicated that the reported adherence to the medication did not influence the blood pressure, and there was the need to determine the factors that cause persistent high blood pressure even when on the medication. Age, symptom frequency, lack of illness complications, and absence of drug side effects among the patients all predicted the probability of medication adherence to improve from low to medium or from medium to high. Medication adherence in hypertension and diabetic patients is not explained by blood pressure, gender, or disease duration.
Kazaure et al. (2017) conducted a study to determine the levels of antihypertensive medication adherence. The study reported that the percentage of those who did not follow the medication prescription was 69.1%. Participants who had been taking antihypertensive medicines for less than 5 years were 1.7 times more likely to be non-adherent than those who had been taking them for more than 5 years (95 % confidence interval: 1.1–2.5). Patients with negative pharmacological side effects were 1.8 substantially more prone to being non – adherent (95% CI: 1.2–2.9). Patients that used alternative medications were 2.0 times more probable to be non-adherent than those who did not (95% confidence interval: 1.2–3.2). Patients who ran out of their drugs before their next clinic session were 8.4 times more likely to be non-adherent (95 % CI: 4.8–14.7) than those who did not. Patients who received less than 5 minutes of counselling were reported to be twice more likely to be non-adherent (95% CI: 1.6–4.3) than those who got more than 5 minutes of counselling. Compared to patients who received less than 5 minutes of counselling, they were reported to be twice more likely to be non-adherent (95% CI: 1.6–4.3) than those who got more than 5 minutes of counselling. Patients who had been in the hospital for more than 3 months were 2.2 times more likely to be non-adherent than those who had been there for less than 3 months (95 % CI: 1.4–3.4). Patients who purchased their medications from a pharmacy and the free markets were twice as likely to be non-adherent than those who purchased their medications from the hospital exclusively (95% confidence interval: 1.6–3.8). Patients who had been in the hospital for more than 3 months were 2.2 times more likely to be non-adherent than those who had been there for less than 3 months (95 % CI: 1.4–3.4).
Ibrahim et al. (2018), reported rates of antihypertensive medication adherence (52.6%) and blood pressure control (36.1%). Religious belief (OR= 0.547, p= 0.03, CI= 0.317-0.943), length of hypertension diagnosis (OR=0.283, p= 0.043, CI= 0.084-0.059), duration of antihypertensive medication for 1-10 years (OR= 7.241, p= 0.033, CI= 0.955-54.896), and taking more than three types of antihypertensive medication (OR= 0.242, p= 0333). Adherence to antihypertensive medication was also linked to blood pressure control and family effectiveness, however the link was not statistically relevant. The study indicated that patients who were older, such as retirees, were more adherent to the medication as they had more time to go to hospitals for check-ups as compared to those who were still employed. Non-adherence was also a result of the high cost of medication as many patients had to pay for their medication.
Osamor and Owumi (2011) and Iloh et al. (2013) discuss the issue of hypertension medication prescription, though they differ in their application. Osamor and Owumi (2011) reported a high adherence rate in patients prescribed a single medication. The study indicated that the bulkiness of the medication increased the rates of non-adherence as the patients mostly did not remember to pack all their medication as opposed to a single therapy. On the contrary, Iloh et al. (2013 reported high adherence in patients with multiple prescriptions. In the study, the authors showed that multiple medications established a sense of concern, and the patients faithfully took their medication to improve their feelings. According to the findings of Iloh et al.’s (2013) study, patients’ beliefs about medication influenced their adherence. Okwuonu et al.’s (2014) findings illustrate that medication adherence is attributed to patient-related challenges.
Olowookere et al. (2015) investigated perceived family support and other factors that influence medication adherence in hypertension patients in a tertiary hospital setting. Olowookere et al. (2015) investigated a total of 420 patients and found that the patients’ average age was 60.6 [+ or −] 11.7 years (range of 21-85 years). There were 206 men (49%) and 214 women (51%) in the group. The majority of respondents were Yoruba (86.2%), married (76.7%), and had only an elementary education (27.6 %). The study further reported that antihypertensive therapy was adhered to by the majority (61%). The belief in a cure (43%), the high cost of therapy (33%), and the experience of side effects are all common causes of poor adherence (27%). Compared to patients with inadequate family support, individuals with high family support had improved adherence (p = 0.05). Poor adherence among these hypertension patients has been linked to a lack of support from family and other factors. Family support in the study is concerned with reminding the patient to take medication and providing financial support for those buying their medication out of pocket.
According to the study by Akunne and Adedapo (2019), a total of 1050 hypertension individuals (females constituted 62% of the study population, with an average age of 60 years). The study found that there was a high level of polypharmacy (87 %) and poor blood pressure control. With an increase in the number of medications prescribed, blood pressure increased (Chi-square = 33.618, p 0.001; r = 18.18, p 0.001). Diuretics are the most commonly given antihypertensive medicine, either as solo therapy or in a fixed-dose combination. Approximately 54% of antihypertensive medication given in daily doses exceeds the daily dosage limit (DDD). The authors further argue that prescription mishaps are predictors of the high non-adherence rates in hypertension patients. They are directly correlated to the cost of medication to be incurred by the patients. Akunne and Adedapo (2019) recommend adherence to the fixed dosage prescription as well as cost-effective drugs to enhance medication adherence in hypertensive patients.
According to Da Silva Barreto et al. (2014), 42.6 % did not follow pharmacological therapy, and 17.7% had limited knowledge of the condition. Complex pharmacological therapy, a lack of understanding about the condition, and dissatisfaction with the healthcare provider were all factors linked to non-adherence. The study indicates that there was no link between beliefs regarding the causation of hypertension and compliance. The study indicates the need for enhanced knowledge about the condition to increased medication adherence among the population. Participants believe that high blood pressure can be treated with both conventional and alternative treatments and that a patient who “feels good” can stop taking antihypertensive medications, according to Osamor and Owumi (2011). Treatment adherence to antihypertensive medication is still low in this Nigerian group, according to the findings.
Okoro and Ngong’s (2012) study sought to determine the factors that result in the adherence or non-adherence of hypertension patients. The study reported a rate of adherence of 85.5%. With a P-value of 0.01, there was a significant relationship between age and adherence, marital status, state of origin, tribe, antihypertensive medication cost, number of drugs prescribed, and age/gender. The study indicated that the patients who were married were more adherent than those who were not. Consequently, older patients and those who had insurance or were financially able were also feeling worse (antihypertensive medication side effects) and feeling better (p = 0.01), which were the prevalent factors for non-adherence. Generally, the study participants showed a high level of adherence. The study also found that their belief significantly influenced patients’ adherence to medication in the diagnosis and the duration of the diagnosis. To improve medication adherence in patients, the authors recommend including patient education about the diagnosis and writing on the medication to remind patients when to take their medication and how many pills there are.
Okeahialiam et al.’s (2011) research was to determine the factors for non-adherence in hypertension patients. A total of 182 hypertensive patients were assessed during the study period. One hundred and twenty-three people (67.6%) followed the prescription to the letter, while 59 people (32.4%) did not. The reasons for non-compliance were numerous. Patients frequently run out of medications before their next session, and in some cases, they misread the instructions. The study reported that morning dosing of medications once daily was recommended. 28 (15.4%) chose the evening dosage. Okeahialiam et al. (2011) further argues that for improved adherence, more effort should be put into health education to realize the importance of taking anti-hypertensive regularly and that blood pressure stabilization does not necessitate withdrawal. Consequently, to avoid patients receiving contradictory instructions, more communication between doctors and pharmacists is required. Osamor and Owumi (2011) agreed further by indicating that patients with appropriate knowledge concerning the condition were more likely to be adherent than those who did not. More recent research, such as Ezeala-Adikaibe et al. (2017) and Ibrahim et al. (2020), also indicted the importance of patient knowledge to improve their reported medication adherence.
From the 18 studies reviewed, they generated similar themes, such as forgetfulness, use of herbal remedies, medication side effects, religious healing, and the cost of medication, feeling better and worse as the factors related to non-adherence. The participants who reported high adherence rates identified social support networks, stability of finances, use of either a single therapy, high formal education or efficient patient education as the underlying factors. Thus, for improved medication adherence among the Nigerian population, the factors that support high adherence should be emphasised.
Table 3: Overview of origin, participants and measuring time point
| Author | Country | Number of participants N | Measuring time points |
| Adisa et al., (2018) | Nigeria | 605 | Not reported |
| Adeoye et al., (2019) | Nigeria | 420 | Not reported |
| Usman (2019) | Nigeria | 237 | 6 months |
| Akunne and Adedapo, (2019). | Nigeria | 1050 | 1 year |
| Kazaure et al. (2017) | Nigeria | 424 | 11 Months |
| Awokola, et al., (2016) | Nigeria | 235 (46% M & 54%F) | 4 months |
| Iloh et al, (2013) | Nigeria | 605 (358 F and 247M). | Two months |
| Iloh and Amadi, (2017) | Nigeria | 140 | 3 months |
| Okoro and Ngong, (2012) | Nigeria | 152 | 6 months |
| Okwuonu et al. (2014) | Nigeria | 252 patients; (143 men and 109 women) | Not disclosed |
| Olowookere et al., (2015) | Nigeria | 420 (206M, 214F). | 8 months |
| Ibrahim et al, (2018) | Nigeria | 302 | 3 months |
| Da Silva Barreto et al. (2014) | Nigeria | 422 | 15 months |
| Oluwole et al., (2019) | Nigeria | 500 | I year |
| Ezeala-Adikaibe et al. (2017) | Nigeria | 436 | Not reported |
| Ayodapo et al. (2020) | Nigeria | 420 | Not reported |
| Okeahialiam et al. (2011) | Nigeria | 182 | Not reported |
Table 4: Overview of non-adherence rates and their contributing factors
| Author and date | Sample size | Age | Duration of hypertension since diagnosis | The educational level of patients | Methods of measuring adherence | Rate of adherence & Non-adherence | Factors contributing to adherence | Factors contributing to non-adherence | Recommendations |
| Adisa et al., (2018) | 605 | Above 18 years | 1 to more than five years | N/A | Morisky Adherence Predictor Scale (2008) | 8.9% adherence
91.1% non-adherence |
Level of education
Multiple medication therapies >5 years of diagnosis |
Forgetfulness
Dose omission Herbal remedies Inability to afford medication Bulkiness of medication Side effects
|
Patient education on the importance of adherence |
| Iloh et al., (2013) | 140 | 18 years and above | >1 to < 3 years | N/A | ordinal scoring system developed by the authors | 42.9% adherence
57.1% non-adherence |
The efforts were given by the clinician to educate the patients | Forgetfulness
A feeling of well-being and cure Lack of funds (to purchase drugs) Advice by spiritual leaders Herbal remedies |
Policy development for reduced medication cost couple with patient education |
| Ezeala-Adikaibe et al., (2019) | 436 | 18years | Not reported | N/A | Morisky Green Score (1986) | 90.1% non-adherence
8.9 adherence |
Knowledge and motivation from the social | Forgetfulness
Reliance on social support Longer years of diagnosis |
Enhanced patient education |
| Iloh and Amadi, (2017) | 140 | ≥18 years | Not reported | N/A | Morisky medication adherence scale (2008) | 42.9% adherence
57.1% non-adherence |
Treatment satisfaction | Lack of continuity of treatment, flexibility, and convenience. | Development of patient-friendly dosages |
| Odusola et al., (2014) | 44 | ≥18 years | 3.3 to 6.1 years | N/A | Morisky Medication Adherence Scale (2008) | 65.7% non-adherence
33.3% adherence |
Belief in the medication efficiency
Fear of the hypertension consequence |
Expectation to be cured
Forgetfulness Pill burden Side effects Low supply of medication |
Enhancement of patient education on hypertension |
| Oluwole et al. (2019) | 500 | ≥18 years | Not reported | N/A | 8-item Morisky Medication Adherence Scale (2008) | Moderate adherence 89.2%, 1% high adherence, 8.8% poor adherence | Treatment satisfaction
Single patients Out of pocket payment scheme |
Side effects
Effectiveness Convenience Married Use of insurance |
Patient education enhancement |
| Ayodapo et al. (2020) | 420 | ≥18 years | At least 6 months | N/A | Morisky Medication Adherence Scale (MMAS-4) (1986) | 61.2% adherence
38.8% adherence |
Awareness about hypertension | Lack of understanding of hypertension condition
Belief of cure
|
Patient awareness creation |
| Adeoye et al. (2019) | 420 | ≥18 years | Not reported | N/A | Morisky Medication Adherence Scale (2008) | 95.9% non-adherence
4.1% adherence |
Advanced formal education | Lack of knowledge
Forgetfulness Medication side effects Belief of cure
|
Enhanced patient education |
| Kazaure et al. (2017) | 424 | Above 18 years | Below 5 and >5 years | N/A | Morisky Green test (1986) | 69.1% non-adherence
30.9%adherence |
Senior servants, buying medicines in hospitals
Counselling for more than five minutes |
being a Junior Civil Servant exhaustion of medicines, buying drugs in private pharmacies total time spent counselling of fewer than five minutes
medication duration of fewer than 5 years medication side effects alternative medication |
Increased time for patient counselling for awareness creation |
| Ibrahim et al. (2018) | 302 | ≥18 years | 1 to 10 years | N/A | Morisky’s Green Medication Adherence Scale (2008) | 52.6% adherence
47.4% non-adherence |
Marriage
Older patients Taking more than 3 pills |
Duration of taking medication
Length of diagnosis
|
Enhancement of the patient medication |
| Da Silva Barreto et al. (2014) | 422 | ≥18 years | Not reported | N/A | Medication Adherence Questionnaire | 57.4% adherence, 42.6% non-adherence | Improved knowledge
Quality healthcare services
|
Use of alternative medication
Belief about the curability of hypertension Dissatisfaction with the therapy |
Patient education enhancement |
| Olowookere et al. (2015) | 420 | ≥18 years | Not reported | N/A | Morisky’s Medication Adherence Scale (2008) | 61% adherence, 39% non-adherence | Higher formal education status
marriage |
Poor family support
High cost of medication Belief of cure Medication side effects |
Inclusion of family in the treatment process |
| Okoro and Ngong, (2012) | 152 | 18 and above | Not reported | N/A | Morisky Medication Adherence Scale (2008) | 75.5% adherence
24.5% non-adherence |
Marriage
Retired or older people |
Medication side effects
Feeling better Cost of medication Detest of the medication Forgetfulness Busy schedule
|
Patient education and reduced cost of medication |
| Akunne and Adedapo, (2019) | 1050 | ≥18 years | Not reported | N/A | Morisky Medication Adherence Scale (2008) | 87% non-adherence
13% adherence |
Accurate prescription
Patient education |
Cost of medication
Controlled blood pressure Knowledge Over prescription |
Reduced cost of medication and patient education enhancement |
| Okeahialiam, et al., (2011) | 182 | ≥18 years | Not reported | N/A | Morisky Medication Adherence Scale (2008) | 67.6% adherence, 32.4% non-adherence | Improved communication between pharmacists and doctors
Patient education |
Ran out of the doses
Misread instructions Preference of the evening doses |
Reduced cost of medication and enhanced communication system |
| Usman et al. (2019) | 237 | ≥18 years | At least 2 years | N/A | Morisky Green Levine (1986) | 36.8% adherence and 63.2% non-adherence | Pharmacist coaching
Taking more than three pills Female and young |
Older patients
Taking a single pill |
Increased advocacy |
| Awokola et al., (2016) | 235 | ≥18 years | 2.2 to 4.2 | N/A | Morisky Medication Adherence Scale (2008) | 59.8% non-adherence
40.2% adherence |
Enhanced patient knowledge on hypertension | Lack of funds, religious healing
Use of herbal remedies Forgetfulness
|
Introduction of insurance covers and patient education enhancement |
Table 5: Literature review matrix
| Author/Year | Title | Study Country/Region | Study Design | Findings | Strength | Weakness |
| Adeoye et al., (2019) | Medication adherence and 24-h blood pressure in apparently uncontrolled hypertensive Nigerian patients | Ibadan – Nigeria | cross-sectional and comparative study | Medication adherence was low, and one-third of the participants had real unmanaged hypertension. Knowledge was found to be an independent predictor of medication adherence but did not influence blood pressure control. For adequate blood pressure control, high medication adherence rather than intermediate adherence, as well as awareness, is required. | The study had a specific study question with an outlined method of study | The results are based on patients attending a single health facility |
| Akintunde and Akintunde, (2015) | Antihypertensive medications adherence among Nigerian hypertensive subjects in a specialist clinic compared to a general outpatient clinic | Cardiology and GOPD Clinic of Ladoke Akintola University of Technology Teaching Hospital, Ogbomoso, Nigeria | Analytical cross-sectional study | The adherence levels varied with the age of the patient, the income of the patient, and the medication prescribed to the patient | The study compared two different clinic settings and thus the validity in the replicability of the result. | The findings cannot be generalized to other study areas |
| Akunne and Adedapo, (2019). | Antihypertensive prescription among black patients without compelling indications: prescription, effectiveness, quality, and cost of medication | Ibadan, Nigeria | Cross-sectional study | Drug adherence is affected by the cost of the medication as many Nigerians lived below 1$ and thus difficult in meeting the basic needs inclusive of the medications. | The study used a large sample size and thus the adequate representation of the population | The study was concentrated in the Ibadan clinic and thus cannot be used to represent the entire Nigerian population, also the duration of hypertension was not assessed. |
| Kazaure et al. (2017) | Factors for nonadherence to antihypertensive drugs among Federal Civil Servants attending health facilities − Abuja, FCT | Abuja | Cross-sectional study | The non-adherence of hypertension patients varied from age, socioeconomic status, counseling of the patient, and where the medication was purchased | The study sample was representative of the population | The findings are based on patients attending one health facility and thus cannot be generalized. |
| Awokola, et al., 2016 | Anti-Hypertensive Medication Adherence in A Primary Care Clinic In South-Western Nigeria: A Study Of Patient-Related Factors | South West Nigeria (Ilesa) | cross-sectional descriptive study | Non-adherence was adduced by forgetfulness, lack of funds, wrong perception of the condition, side effects of the medication, use of herbal medication, and the belief in spiritual healing | The study focused only on patient-related factors | The results cannot be generalized in other states |
| Iloh et al, (2013) | Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern Nigeria. | Abia State, Eastern Nigeria. | Cross-sectional study | Non-adherence was proffered by lack of adequate funds, forgetfulness, feeling well, a proclamation of the spiritual leader for healing, and the use of herbal medicines. | The sample size was mathematically calculated and the study involved only patients with hypertension and not any other comorbidity such as diabetes | The findings cannot be generalized to other states |
| Adisa et al., (2018) | Treatment adherence and blood pressure outcome among hypertensive out-patients in two tertiary hospitals in Sokoto, Northwestern Nigeria | Sokoto, Northwestern Nigeria | Cross-sectional study | Forgetfulness, medication side effects, feeling better, | The study utilised random sampling and thus participation inclusivity | The study focussed on two tertiary facilities and thus cannot be generalized, researcher bias |
| Iloh and Amadi, 2017 | Treatment satisfaction, medication adherence, and blood pressure control among adult Nigerians with essential hypertension | Abia State, South-East Nigeria | Descriptive study
Interviewer administered questionnaire |
There is variability between medication adherence, patient satisfaction, and blood pressure control. | The study provides insights on the interaction of factors that affects the patient’s wellness | The study focussed on the patients being followed up and thus not a reflection of the entire hypertensive population |
| Okoro and Ngong, 2012 | Assessment of patient’s antihypertensive medication adherence level in non-comorbid hypertension in a tertiary hospital in Nigeria | Uaiduguri Teaching Hospital (UMTH), Maiduguri, Borno State, Nigeria | Cross-sectional study | Medication non-adherence was caused by forgetfulness, feeling well, medication side effects, medication bulkiness, dislike of the medication, and discontinuation occurred when they felt worse when on medication | The study involved only hypertensive patients | The study used a self-reported questionnaire which is compromised by the honesty of the patient |
| Odusoal et al., 2014 | Perceptions of inhibitors and facilitators for adhering to hypertension treatment among insured patients in rural Nigeria: a qualitative study. | Kwara state Nigeria Ogo Oluwo hospital. | Qualitative study | Low adherence is attributed to financial constraints, belie that they care be cured, forgetfulness, high pill burden, and medication side effects | The study focused on the patients’ related factors as well as healthcare influence | The findings are based on a single region and helath facility and thus cannot be generalized to represent the entire nation |
| Olowookere et al., (2015) | Perceived family support and factors influencing medication adherence among hypertensive patients attending a Nigerian tertiary hospital | Medical Outpatient Clinic of Federal Medical Centre Owo, Ondo State, Nigeria | Cross-sectional study | Non-adherence was caused by the high cost of medication, belief that the condition is curable, and medication side effects. Social support increased the levels of adherence | The study included the role of the family in the determining non-adherence | The study was concentrated to a health facility and thus can not be applied to the general population |
| Osamor and Owumi, (2011) | Factors associated with treatment compliance in hypertension in southwest Nigeria. | Idikan community, Ibadan South-western Nigeria | Community-based survey
Focus-group discussions (FGDs) |
The patient who reported non-adherence were adduced by forgetfulness, feeling better, medication side effects, busy schedule, and lack of financial capability to purchase medication | The study used two quantitative methods and thus the ability to compare the findings and draw a reliable conclusion. | The study is based on one community and also reliant on the patient-reported information |
| Oluwole et al., (2019) | Medication adherence and patient satisfaction among hypertensive patients attending an outpatient clinic in Lagos University Teaching Hospital, Nigeria | Lagos University Teaching Hospital (LUTH), Nigeria | Descriptive cross-sectional study | There was low adherence among the participants. High adherence was related to patient satisfaction | The study is reflective of the patient’s perspective | The study was involved patients of a single clinic and thus cannot represent the general population |
| Odiase and Ogbemudia, (2019) | Predictors of non-adherence to antihypertensive medications among stroke survivors in Benin City Nigeria | Benin Teaching Hospital, Benin City, Southern Nigeria | Cross-sectional study | Medication adherence is not influenced by marital status. Female and illiterate patients are more likely to be non-adherent | The study assed different factors and thus offering reliable findings | It was a single hospital-based and thus cannot be replicated in the general population in other regions |
| Okeahialiam et al., (2011) | Adherence and preference issues in anti-hypertensive therapy: experience from a private medical facility in Jos, Nigeria | Jos, Nigeria | Cross-sectional study | Many patients ran out of their prescribed medication before their next clinic, they preferred evening dosages as compared to the morning prescribed and some patients misunderstood the prescription | The findings reflect patient felt concerns | Hospital-based study and entailing a single region and thus cannot be generalized |
| Ibrahim et al., (2018) | Blood pressure control and its associated factors among hypertensive patients in a federal teaching hospital, Ido- Ekiti, Southwest Nigeria | Family Practice Clinic of Ahmadu Bello University Teaching Hospital, Zaria, (ABUTH, Zaria) | Analytical cross-sectional study | The adherence to medication correlated with the controlled blood pressure. Married, older, and economically stable patients were more adherent than the young and those with a busy schedule. | The study evaluated patient-related aspects that can affect adherence | Recall Bias
The study is not a reflection of the general population as it has specific patients being followed up
|
| Ezeala-Adikaibe et al.,2017 | Factors associated with medication adherence among hypertensive patients in a tertiary health center: a cross-sectional study. | Enugu Nigeria | Cross-sectional descriptive study | Many patients forgot to pack their medication. Non-adherence also increased with dependence and the rates of depression reported by the patient | The study focused on determining the cause of non-adherence | Hospital-based study and thus cannot be generalized. |
| Ayodapo et al., 2020 | Patient education and medication adherence among hypertensives in a tertiary hospital, South-Western Nigeria | Federal Medical Centre (FMC), Ido-Ekiti
South Western Nigeria |
Descriptive cross-sectional study | Poor knowledge about hypertension correlated with poor medication adherence, consequently a busy schedule in the high class contributed to the missed pills | The study entailed a large population that is representative of the population | The study only patients attending hospital clinics |
| Da Silva Barreto et al. (2014) | To explore factors influencing nonadherence among the Nigerian hypertension population. | Major Nigerian referral hospitals. | Descriptive cross-sectional study | Poor patient knowledge about hypertension management. Number of medication regimens. | The included relatively large number of participants, 422 hypertensive patients | Perception of patients or health care providers were not included in the collected data. |
Table 6: CASP Checklist Summary
| Author/ Year | Clear Aim of the study | Appropriate methodology used | Appropriate research design | Appropriate recruitment strategy | Appropriate data collection methods | Researcher participant relationship considered | Ethical concerns considered | Rigorous data analysis | Clear study findings | Value of the research |
| Adeoye et al., (2019) | YES | YES | YES | YES | YES | NO | YES | Lack of sufficient information to assess | YES | Valuable |
| Akintunde and Akintunde, (2015) | YES | YES | YES | YES | YES | Inconclusive | YES | YES | YES | Valuable |
| Akunne and Adedapo, (2019). | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Kazaure et al. (2017) | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Awokola, et al., 2016 | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Iloh et al, (2013) | YES | YES | YES | YES | YES | YES | YES | YES | Valuable | |
| Adisa et al., (2018) | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Iloh and Amadi, 2017 | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Okoro and Ngong, 2012 | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Okwuonu et al., 2014 | YES | YES | YES | YES | YES | Yes | YES | YES | YES | Valuable |
| Olowookere et al., (2015) | YES | YES | YES | YES | YES | YES | YES | YES | YES | Valuable |
| Osamor and Owumi, (2011) | YES | YES | YES | YES | YES | YES | YES | NO | YES | Valuable |
| Oluwole et al., (2019) | YES | YES | YES | YES | YES | NO | YES | NO | YES | Valuable |
| Odiase and Ogbemudia, (2019) | YES | YES | YES | YES | YES | YES | YES | YES | YES | Valuable |
| Okeahialiam et al., ((2011)) | YES | YES | YES | YES | YES | NO | YES | YES | YES | Valuable |
| Ibrahim et al., 2020 | YES | YES | YES | YES | YES | YES | YES | NO | YES | Valuable |
| Ezeala-Adikaibe et al.,2017 | YES | YES | YES | YES | YES | YES | YES | YES | YES | Valuable |
| Ayodapo et al., 2020 | YES | YES | YES | YES | YES | YES | YES | YES | YES | Valuable |
Discussion
Introduction
The primary purpose of the present systematic review of literature was to determine the rates of medication nonadherence among Nigerian adults with hypertension and the primary factors that influence the occurrence of such trends. Specifically, this study identified four key factors influencing medication nonadherence among the hypertension patients: they include social and economic factors, health care system and time factors, therapy-related factors and the patients related factors. The chapter provides a summary of the results generated during the systematic literature review process, discusses the outlined findings by comparing and contrasting them to those presented in the previous literature leading to the creation of new knowledge, highlights major limitations of the present study and recommendations for both future research and health care practice in addition to the general conclusion of the whole research.
Summary of the Results
The initial literature search process led to the identification of 369 articles from two databases, PubMed and EMBASE. However, only 18 studies met all inclusion criteria and were selected for this review. Outcomes from the present systematic review of literature show that the Nigerian patients living with hypertension have varying rates of medication nonadherence depending on the factors influencing development of such unhealthy behavior. For example, Ibrahim et al. (2018) and Usman et al. (2019) reported medication nonadherence rates of 52.6% and 60.8% among the Nigerian hypertension patients, respectively, with both of the studies establishing that the adherence rates are largely influenced by the duration of diagnosis. Moreover, Da Silva Barreto et al. (2014), Gabriel et al., (2017), Olowookere et al. (2015) and Raimi (2017) reported high nonadherence rates among the elderly patients (63.5% on average) compared to Ezeala-Adikaibe et al., (2019), Okeahialiam, et al., (2011), Okoro and Ngong, (2012) who reported low nonadherence rates among young adults aged 18-35 years (44.8% on average). Based on these outcomes, it is justifiable to note that medication nonadherence rates worsen with the increase in age.
Generally, the outcomes from systematic review of literature show that adherence rates to long-term pharmacotherapies for hypertension treatment often averages between 50% and 60% irrespective of the patient demographics, regimen or the type of adherence measurement criteria used. According to Ezeala-Adikaibe et al., (2019), Gabriel et al. (2017) and Iloh et al., (2013), poor or lack of medication adherence is one of the key factors influencing the occurrence of poor blood pressure control among the hypertension patients. Therefore, it is justifiable to note that lack or poor adherence to hypertension medication on a long-term basis often severely compromise the efficiency of treatment, making it a critical issue both from the quality of life and patient outcomes, and the health outcomes of the involved patients. Even though the selected for review identified varying types of factors influenced in the increasing nonadherence rates among hypertension patients, the factors can be generalized into four key groups. Specifically, Adeoye et al. (2019), Da Silva Barreto et al. (2014), Gabriel et al. (2017) and Iloh et al., (2013) identified ineffective social support services and socioeconomic factors such as medication cost as key influencers of medication nonadherence among the hypertension patients; all can be generalized into a “social and economic factors” group.
The second group of medication nonadherence factors “health care team and system” was reported in the studies by Ayodapo et al. (2020), Ibrahim et al. (2018), Odusola et al., (2014) and Ozumba and Ndukwi (2021) which identified lack of clear communication and limited time spent by the health care providers when explaining the disease and treatment process to the patients as key influencers of poor adherence to medication among the hypertension patients. Additionally, the therapy-related factors reported in the studies by Ezeala-Adikaibe et al., (2019), Olowookere et al. (2015) and Raimi (2017) include side effects of hypertension medication on the patients in addition to the complexity of medication regimen, such as the number of medications and frequency of dosing. Furthermore, Okeahialiam, et al., (2011), Okoro and Ngong, (2012) and Usman et al. (2019) identified patient-related factors such as health beliefs, emotional state and health literacy as some of the key influencers of low adherence rates among the Nigerian patients living with hypertension.
Discussion
Poor medication adherence is a major problem reported among the Nigerian hypertensive patients and has been established to have major impacts on the clinical outcomes, leading to substantial worsening of patient quality of life, increased cost of health care and death (Ezeala-Adikaibe et al., 2019; Iloh et al., 2013; Ozumba and Ndukwi, 2021). Correspondingly, Iloh and Amadi, (2017) noted that the increasing number of medications administered to patients living with hypertension has significantly led to high incidences of nonadherence, which has seriously undermined the benefits of current medical care practice for people living with hypertension. Evidence from all of the studies included in this systematic review of literature shows that nonadherence to hypertension medication facilitates reduction in the levels of treatment benefits in addition to distorting the assessment of the treatment efficiency.
According to Ayodapo et al. (2020), Odusola et al., (2014) and Raimi (2017), unawareness of physicians about the fact that patients living with hypertension are not taking drugs as prescribed may lead to mistreatment by attributing uncontrolled blood pressure to the inefficiency of the medication leading to unnecessary increase in dosage, changing or adding of another medication. Corresponding arguments were also provided in the previous studies by Akunne and Adedapo (2019), Boima et al. (2015) and Gakidou et al. (2017) where it was noted that ineffectiveness of hypertension treatment and disease progression as a result of nonadherence may lead to the development of poor patient outcomes, hospitalizations, disease complications, increased visits to the emergency department, and death. According to the World Health Organisation (2002), increasing the effectiveness of adherence interventions has greater impacts on the health population compared to any other improvement approach specific to the medical treatments. From a general perspective, the outcomes from the present systematic review of literature are consistent with those presented in the previous studies about hypertension medication nonadherence based on the patients’ age.
In a study by Okwuonu et al. (2014) involving 100 patients with hypertension (aged 55-85 years), nonadherence was reported among 49 patients (55.1%) during the first follow-up and 55 patients (69.6%) during the second follow-up period conducted after 3 months of discharge. Similarly, one of the studies included in this systematic review of literature involving 237 Nigerian patients with hypertension, reported an overall medication nonadherence rate of 39.2%, with high adherence levels being observed among hypertensive patients who were administered with three medication and among those who got pharmacist coaching. Based on these outcomes, it is justifiable to note that low medication adherence is a major factor limiting the efficiency of hypertension treatment process, especially among the elderly hypertensive patients who are receiving polypharmacy.
Similar to the results presented in the previous studies by Adeyemo et al. (2013), Amadi (2013) and Forouzanfar et al. (2017), evidence from the studies included in the present systematic review of literature shows that there is a positive correlation between the increasing number of drugs prescribed at the hospital discharge and nonadherence rates as most of the patients (specifically the elderly) are often not able to understand the purpose of each medication administered to them. Therefore, there is need to simplify the drug regimens, reduce pill number in addition to improved patient education about the purpose of each medication prescribed to them as major strategies for lowering nonadherence rates among the adult population living with hypertension in Nigeria.
The present systematic review of literature has also established that there is a negative association between the patient demographic factors and hypertension nonadherence rates, with key factors being age and gender. Similar to the evidence presented in the previous studies by Odiase and Ogbemudia (2019), Okubadejo et al. (2019) and Osamor and Owumi (2011), the present review has established that male patients often exhibit higher levels of hypertension nonadherence compared to their female counterparts, with the trend being more severe among the male patients involved in excessive consumption of alcohol. However, Okoro and Ngong, (2012) and Olowookere et al. (2015) reported no significant difference in the adherence rate of hypertension patients from the perspective of their age and gender, contrary to the findings from the present study. Therefore, detailed comparison of these findings leads to the development of a general knowledge that patient demographic alone such as gender and gender are not the key determinants of medication adherence among patients living with hypertension and that other factors such as patient education, health care system and number of dosage regimens are also playing an important role in determining the nonadherence rates.
In a multivariate model for combined population conducted by Forouzanfar et al. (2017), low levels of hypertension medication adherence were linked with different factors such as lack of long-term housing, not belonging to a hypertension or cardiovascular disease support group, excessive alcohol and substance use in addition to significant side effects of the medication. Even though significant number of these findings were also reported in the present systematic literature review, this study failed to develop a comprehensive relationship between gender-based drug and substance abuse and hypertension nonadherence rates within the Nigerian population. The results from the present review show that future hypertension medication adherence studies would be informed and strengthened by gender-stratified analysis. The existence of consistent gender-based disparities in medication adherence in such studies would therefore suggest that the adherence improving interventions should be gender-specific.
Similar to the prior studies, such as Akinlua et al. (2018), Akintunde and Akintunde (2015), Akunne and Adedapo (2019) and Boima et al. (2015), the present systematic literature review, specifically evidence from the studies such as Gabriel et al., 2017, Okeahialiam, et al., (2011) and Usman et al. (2019), established that the severity of disease factor is among the key factors for adherence among the Nigerian patients with hypertension. According to Adeyemo et al. (2013) and Akintunde and Akintunde (2015), hypertension is largely asymptomatic in nature; therefore, hypertensive patients experiencing additional chronic diseases, including those with hypertension-related complications and longer duration of hypertension were more likely to receive regular care, provided with more knowledge about the importance of medication adherence leading to the development of positive habits required for consistent taking of the hypertensive medications. Therefore, patients within such groups reported higher levels of hypertension medication adherence.
Even though the present review did not specifically assess the impacts of community management on hypertension medication adherence, previous studies by Odiase and Ogbemudia (2019) and Oluwole et al. (2019) reported that hypertensive patients who undergo community management were nonadherent to the antihypertensive medication regimens. However, the findings from these previous studies are consistent with the results obtained from the present systematic review of literature as both established that patients with no regular clinical and blood pressure checks in addition to those unable to effectively control their blood pressure showed higher rates of nonadherence to their medication regimens. Therefore, there is need for health care practitioners caring for hypertensive patients to improve the standardized management and health education for their patients as a strategy for improving medication adherence.
Limitations of the Study
Even though the present systematic review of literature was able to achieve its key purpose of identifying the nonadherence rates among hypertension patients and key factors influencing development of such trends within the Nigerian population, it still has specific limitations which should be addressed by future researchers in this area. Although the present systematic review employed abroad inclusion criteria, only 18 studies were found to be eligible and included in the evidence synthesis process, hence limiting the comprehensiveness of newly developed knowledge. Furthermore, most of the studies included in this review were observational, with very few being randomised controlled trials. Additionally, all of the included studies in this review failed to provide a clear and consensus definition of adherence and polypharmacy. Therefore, studies about the hypertension medication administration were heterogenous in nature in relation to the populations involved and the registered outcomes. However, this study was still able to register strongest association between patient demographics and hypertensive medication nonadherence. Additionally, overreliance on the studies from previously published research papers limited the ability of the present study to generate new evidence that is unique and different from those presented in the existing literature.
Recommendations for Future Research
Completion of this study has led to the identification of key areas that need further research in order to comprehensively understand and address the factors influencing the occurrence of high nonadherence rates among the Nigerian adult patients with hypertension. Even though demographic characteristics of the patients had been reported in this study to play an important role in determining their hypertension medication adherence rate, there is still limited knowledge about the precise factors influencing high nonadherence among males compared to females. Therefore, future research in this area should focus on identifying and reporting the primary factors influencing the occurrence of medication adherence disparity based on the patients’ gender among other demographic characteristics. Furthermore, further research should compare and contrast the medication adherence rates among the Nigerian hypertensive patients based on their geographic location, such as rural and urban setting. Moreover, extensive research should be conducted in order to assess efficiency of different hypertension medication so as to identify the more preferable medication for the Nigeran patients living with hypertension.
Implications of the Study
The present study has established that medication nonadherence is among the major factors limiting proper treatment and management of hypertension patients from the Nigerian population, with key factors such as number of medication and patient education playing an important role. Therefore, the outcomes from this study can be used to suggest that interventions for improving adherence can be most effective and lead to generation of positive results if delivered in the form of medication review, with the primary ai of prescription regime simplification in addition to providing people living with hypertension detailed information about the importance of each medication administered to them. Even though not provided in much detail, the present study has established that there is a positive association between patient demographic characteristics, such as age and gender, on their adherence levels to the hypertension medication. Therefore, these outcomes suggest the need to develop tailored hypertension management strategies, including medication administration process, based on the demographic characteristics of the patients.
Conclusion
The primary purpose of the present study was to systematically review existing literature in order to determine medication nonadherence rates among hypertension patients from the Nigerian adult population. The analysis led to the identification of four key themes describing these factors; they include social and economic factors, health care team and system, therapy-related factors as well as the patient-related factors such as health beliefs, emotional state and health literacy. The present review goes beyond the findings of the previous systematic review of literature as it primarily involved the collection and analysis of evidence presented in the prior studies within the Nigerian hypertension patient population, an area that has not been extensively researched by existing studies. Results obtained from this study support the existing evidence from the previous studies that health-related knowledge, number of dosage or medication regimen in addition to the cognitive impairment have significant impacts on the medication adherence among hypertensive patients. Nonetheless, reported findings in this study add uncertainty to the existing notion that medication compliance aids are efficient in reducing nonadherence rates, hence suggesting the need for further research in order to identify and assess efficiency of other forms of medication adherence strategies for the hypertensive patients.
References
Abegaz, T. M., Shehab, A., Gebreyohannes, E. A., Bhagavathula, A. S., and Elnour, A. A. 2017. Nonadherence to antihypertensive drugs: A systematic review and meta-analysis. Medicine, 96(4), e5641-e5641. https://doi.org/10.1097/MD.0000000000005641
Adeoye, A.M., Adebiyi, A.O., Adebayo, O.M. and Owolabi, M.O., 2019. Medication adherence and 24-h blood pressure in apparently uncontrolled hypertensive Nigerian patients. Nigerian Postgraduate Medical Journal, 26(1), p.18.
Adeloye, D., Basquill, C., Aderemi, A. V., Thompson, J. Y., and Obi, F. A. 2015. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens, 33(2), 230-242. https://doi.org/10.1097/hjh.0000000000000413
Adeyemo, A., Tayo, B.O., Luke, A., Ogedegbe, O., Durazo-Arvizu, R. and Cooper, R.S., 2013. The Nigerian antihypertensive adherence trial: a community-based randomized trial. Journal of Hypertension, 31(1), pp.201–207.
Adisa, R., Ilesanmi, O.A. and Fakeye, T.O., 2018. Treatment adherence and blood pressure outcome among hypertensive out-patients in two tertiary hospitals in Sokoto, Northwestern Nigeria. BMC Cardiovascular Disorders, 18(1), pp.1-10.
Akinlua, J.T., Meakin, R., Bashir, I. and Freemantle, N., 2018. Beliefs about hypertension among primary health care workers and clients in Nigeria: a qualitative study. PloS One, 13(12), p. e0209334.
Akinlua, J.T., Meakin, R., Umar, A.M. and Freemantle, N., 2015. Current prevalence pattern of hypertension in Nigeria: a systematic review. PloS One, 10(10), p.e0140021.
Akintunde, A.A. and Akintunde, T.S., 2015. Antihypertensive medication adherence among Nigerian hypertensive subjects in a specialist clinic compared to a general outpatient clinic. Annals of Medical and Health Sciences Research, 5(3), pp.173-178.
Akunne, O.O. and Adedapo, A.D.A., 2019. Antihypertensive prescription among black patients without compelling indications: prescription, effectiveness, quality, and cost of medication. BMC Health Services, 19(1), pp.1-8.
Aronow, W. S. 2017. Lifestyle measures for treating hypertension. Archives of medical science: AMS,
13(5), 1241-1243. https://doi.org/10.5114/aoms.2017.68650
Awokola, B., Amusa, G., Isiguzo, G. and Abioye-Kuteyi, E., 2016. PS 17-72 anti-hypertensive medication adherence in a primary care clinic in South-Western Nigeria: a study of patient-related factors. Journal of Hypertension, 34, p. e494.
Ayodapo, A.O., Elegbede, O.T., Omosanya, O.E. and Monsudi, K.F., 2020. Patient education and medication adherence among hypertensives in a tertiary hospital, South-Western Nigeria. Ethiopian Journal of Health Sciences, 30(2), pp.11-19.
Bastian, H., 1994. The power of sharing knowledge: consumer participation in the Cochrane collaboration. Oxford: UK Cochrane Centre.
Benziger, C. P., Roth, G. A., and Moran, A. E. 2016. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart, 11(4), 393-397. https://doi.org/10.1016/j.gheart.2016.10.024
Boima, V., Ademola, A.D., Odusola, A.O., Agyekum, F., Nwafor, C.E., Cole, H., Salako, B.L., Ogedegbe, G. and Tayo, B.O., 2015. Factors associated with medication nonadherence among hypertensives in Ghana and Nigeria. International Journal of Hypertension, 2015, pp.1-8.
Burnier, M. 2017. Drug adherence in hypertension. Pharmacol Res, 125(Pt B), 142-149. https://doi.org/10.1016/j.phrs.2017.08.015
Burns, P. B., Rohrich, R. J., and Chung, K. C. 2011. The levels of evidence and their role in
Evidence-based medicine. Plastic and reconstructive surgery, 128(1), 305-310. https://doi.org/10.1097/PRS.0b013e318219c171
Cerigo, H. and Quesnel-Vallée, A., 2020. Systematic mixed studies reviews: leveraging the literature to answer complex questions through the integration of quantitative and qualitative evidence. International Journal of Public Health, 65(1), pp.699-703.
Cleary, P. and Neumann, D., 2009. The challenges of primary sources, collaboration, and the K-16 Elizabeth Murray Project. The History Teacher, 43(1), pp.67-86.
da Silva Barreto, M., Reiners, A.A.O. and Marcon, S.S., 2014. Knowledge about hypertension and factors associated with the non-adherence to drug therapy. Revista latino-americana de-enfermagem, 22(3), p.491.
DiMatteo, M. R., Haskard-Zolnierek, K. B., and Martin, L. R. 2012. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev, 6(1), 74-91.
Dubben, H.H. and Beck-Bornholdt, H.P., 2005. A systematic review of publication bias in studies on publication bias. BMJ, 331(7514), pp.433–434.
Ezeala-Adikaibe, B.A., Mbadiwe, N., Okudo, G., Nwosu, N. and Nwobodo, N., 2017. Factors associated with medication adherence among hypertensive patients in a tertiary health center: a cross-sectional study. Arch Community Med Public Health, 3(1), pp.024-031.
Forouzanfar, M.H., Liu, P., Roth, G.A., Ng, M., Biryukov, S., Marczak, L., Alexander, L., Estep, K., Abate, K.H., Akinyemiju, T.F… and Ali, R., 2017. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. Jama, 317(2), pp.165-182.
Gakidou, E., Afshin, A., Abajobir, A.A., Abate, K.H., Abbafati, C., Abbas, K.M., Abd-Allah, F., Abdulle, A.M., Abera, S.F., Aboyans, V. and Abu-Raddad, L.J., 2017. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390(10100), pp.1345-1422.
Gascón, J.J., Sánchez-Ortuño, M., Llor, B., Skidmore, D. and Saturno, P.J., 2004. Treatment compliance in hypertension study group. Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract, 21, pp.125-130.
Green, S., Higgins, J.P., Alderson, P., Clarke, M., Mulrow, C.D. and Oxman, A.D., 2011. Chapter 1: introduction. [Online] Available at: www.handbook.cochrane.org [Accessed 07/03/21].
Hewitt, C.E., Mitchell, N. and Torgerson, D.J., 2008. Listen to the data when the results are not significant. BMJ, 336(7634), pp.23-25.
Ibrahim, O.A., Olaniyan, F.A., Sule, A.G. and Ibrahim, B.Y., 2018. Socio-demographic and clinical factors affecting adherence to antihypertensive medications and blood pressure control among patients attending the family practice clinic in a tertiary hospital in northern Nigeria. Nigerian Journal of Family Practice, 9(1), pp.39-49.
Ibrahim, A.O., Agbesanwa, T.A., Shabi, O.M., Omosanya, O.E., Ismail, W.O. and Deji-Dada, O.O., 2020. Blood pressure control and its associated factors among hypertensive patients in federal teaching hospital, ido-ekiti, Southwest Nigeria. Archives of Community Medicine and Public Health, 6(2), pp.167-173.
Iloh, G.U. and Amadi, A.N., 2017. Treatment satisfaction, medication adherence, and blood pressure control among adult Nigerians with essential hypertension. International Journal of Health & Allied Sciences, 6(2), p.75.
Iloh, G.U., Ofoedu, J.N., Njoku, P.U., Godswill-Uko, E.U. and Amadi, A.N., 2013. Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern Nigeria. African Journal of Primary Health Care and Family Medicine, 5(1), pp.1-6.
Jimmy, B., and Jose, J. 2011. Patient medication adherence: measures in daily practice. Oman medical journal, 26(3), 155-159. https://doi.org/10.5001/omj.2011.38
Lee, S. Q., Raamkumar, A. S., Li, J., Cao, Y., Witedwittayanusat, K., Chen, L., and Theng, Y. L. 2018. Reasons for Primary Medication Nonadherence: A Systematic Review and Metric Analysis. J Manag Care Spec Pharm, 24(8), 778-794. https://doi.org/10.18553/jmcp.2018.24.8.778
Musini, V. M., Gueyffier, F., Puil, L., Salzwedel, D. M., and Wright, J. M. 2017. Pharmacotherapy for hypertension in adults aged 18 to 59 years. Cochrane Database Syst Rev, 8(8), Cd008276. https://doi.org/10.1002/14651858.CD008276.pub2
National Institute for Health and Care Excellence (NICE) 2009. ‘Medicines adherence:
Involving patients in decisions about prescribed medicines and supporting adherence’, Available Online: https://www.nice.org.uk/guidance/cg76/resources/medicines-adherence-involving-patients-in-decisions-about-prescribed-medicines-and-supporting-adherence-pdf-975631782085, [Accessed On: 17 Apr 2021]
National Institute for Health and Care Excellence (NICE) 2019. ‘Hypertension in adults: diagnosis and management’, Available Online: https://www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-management-pdf-66141722710213, [Accessed On: 16 Apr 2021]
Odiase, F.E. and Ogbemudia, J.E., 2019. Predictors of nonadherence to antihypertensive medications among stroke survivors in Benin City Nigeria. Sub-Saharan African Journal of Medicine, 6(3), p.122.
Odili, A.N., Chori, B.S., Danladi, B., Nwakile, P.C., Okoye, I.C., Abdullahi, U., Nwegbu, M.N., Zawaya, K., Essien, I., Sada, K. and Ogedengbe, J.O., 2020. Prevalence, awareness, treatment, and control of hypertension in Nigeria: data from a nationwide survey 2017. Global Heart, 15(1), pp.123-131.
Odusola, A.O., Hendriks, M., Schultsz, C., Bolarinwa, O.A., Akande, T., Osibogun, A., Agyemang, C., Ogedegbe, G., Agbede, K., Adenusi, P. and Lange, J., 2014. Perceptions of inhibitors and facilitators for adhering to hypertension treatment among insured patients in rural Nigeria: a qualitative study. BMC health services research, 14(1), pp.1-16.
Okeahialam, B.N., 2011. Adherence and preference issues in anti-hypertensive therapy: experience from a private medical facility in Jos, Nigeria. Journal of Medicine in the Tropics, 13(1), pp.45-57.
Okoro, R.N. and Ngong, C.K., 2012. Assessment of patient’s antihypertensive medication adherence level in non-comorbid hypertension in a tertiary hospital in Nigeria. Int J Pharm Biomed Sci, 3(2), pp.47-54.
Okubadejo, N.U., Ozoh, O.B., Ojo, O.O., Akinkugbe, A.O., Odeniyi, I.A., Adegoke, O. and Agabi, O.P., 2019. Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clinical Hypertension, 25(1), pp.1-9.
Okwuonu, C.G., Ojimadu, N.E., Okaka, E.I. and Akemokwe, F.M., 2014. Patient-related barriers to hypertension control in a Nigerian population. International Journal of General Medicine, 7(1), p.345.
Olowookere, A.J., Olowookere, S.A., Talabi, A.O., Etonyeaku, A.C., Adeleke, O.E. and Akinboboye, O.O., 2015. Perceived family support and factors influencing medication adherence among hypertensive patients attending a Nigerian tertiary hospital. Annals of Tropical Medicine and Public Health, 8(6), p.241.
Oluwole, E.O., Osibogun, O., Adegoke, O., Adejimi, A.A., Adewole, A.M. and Osibogun, A., 2019. Medication adherence and patient satisfaction among hypertensive patients attending an outpatient clinic in Lagos University Teaching Hospital, Nigeria. Nigerian Postgraduate Medical Journal, 26(2), p.129.
Oparil, S., Acelajado, M. C., Bakris, G. L., Berlowitz, D. R., Cífková, R., Dominiczak, A. F., Grassi, G., Jordan, J., Poulter, N. R., Rodgers, A., and Whelton, P. K. 2018. Hypertension. Nat Rev Dis Primers, 4, 18014-18014. https://doi.org/10.1038/nrdp.2018.14
Osamor, P.E. and Owumi, B.E., 2011. Factors associated with treatment compliance in hypertension in southwest Nigeria. Journal of Health, Population, and Nutrition, 29(6), p.619.
Pollock, A. and Berge, E., 2018. How to do a systematic review. International Journal of Stroke, 13(2), pp.138-156.
Ranganathan, P. and Aggarwal, R., 2020. Study designs: part 7–Systematic reviews. Perspectives in Clinical Research, 11(2), p.97.
Schardt, C., Adams, M.B., Owens, T., Keitz, S. and Fontelo, P., 2007. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Medical Informatics and Decision Making, 7(1), pp.1-6.
Selçuk, A. A. 2019. A Guide for Systematic Reviews: PRISMA. Turkish archives of otorhinolaryngology, 57(1), 57-58. https://doi.org/10.5152/tao.2019.4058
Shea, B., Dubé, C. and Moher, D., 2001. Assessing the quality of reports of systematic reviews: the QUOROM statement compared to other tools. Systematic Reviews in Health Care: Meta-Analysis in Context, 2(1), pp.122-39.
Straka, I., Minár, M., Gažová, A., Valkovič, P., and Kyselovič, J. 2018. Clinical aspects of adherence to
pharmacotherapy in Parkinson disease: A PRISMA-compliant systematic review. Medicine, 97(23), e10962-e10962. https://doi.org/10.1097/MD.0000000000010962
Suri, H., 2020. Ethical considerations of conducting systematic reviews in educational research. In: Systematic Reviews in Educational Research. Wiesbaden: Springer, pp.98-103.
Usman, M.N., Umar, M.D., Idris, F.A. and Abdullahi, Y., 2019. Medication adherence and its associated factors among hypertensive patients in a tertiary health facility in Minna, North central Nigeria. Archives of Clinical Hypertension, 5(1), pp.003-007.
Vergnes, J.N., Marchal-Sixou, C., Nabet, C., Maret, D. and Hamel, O. 2010. Ethics in systematic reviews. Journal of Medical Ethics, 36(12), pp.771–774.
World Health Organisation, 2002. The world health report 2002: Reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organisation.
Yin, R. K., 2014. Case study research design and methods. Thousand Oaks, CA: Sage.
Zhou, D., Xi, B., Zhao, M., Wang, L., and Veeranki, S. P. 2018. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III Linked Mortality Study. Scientific reports, 8(1), 9418-9418. https://doi.org/10.1038/s41598-018-27377-2